Q. I recently heard that Sandra Day O’Connor, the first female Supreme Court Justice, announced that she has Alzheimer’s disease. Her son explained how she overcame so many obstacles in her life that she was convinced that she could power through Alzheimer’s as well, but sadly you can’t. He describes how she still loves having visitors and that she can still carry on a wonderful conversation, but short-term memory is a challenge these days.
Alzheimer’s is prevalent in my family on my father’s side, unfortunately. I had several relatives die from it before I was born, and my brother was recently diagnosed. Since he was never married or never had children, I am expecting to contribute to caregiving duties for him in the future. What is the progression of the disease like, how long does each stage typically last, and what type of care is needed at each stage? What happens when the disease becomes more than I can handle as a caregiver? Thanks for your help!
A. I’m very sorry to hear about your brother’s diagnosis. As you know, the discovery that you or a loved one has Alzheimer’s disease is always a very traumatic emotional experience. Whether you’re a family member, a caregiver, or someone with the condition, this progressive disease will impact your daily life in innumerable ways that are hard to imagine unless you have lived through it.
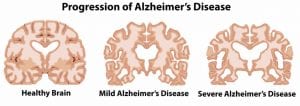
Currently, more than 50 million people in the world suffer from the dementia of Alzheimer’s diseas and, unfortunately, the number is expected to rise above 150 million by 2050. Alzheimer’s is a progressive disease, so it’s important to understand the stages of Alzheimer’s and what to expect.
The 3-Stage Scale
The three-stage scale is one scale that many doctors use to describe the typical progression of Alzheimer’s disease:
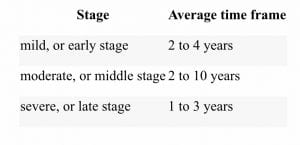
But there is no universally agreed upon staging system, so healthcare providers may use the one that they are most familiar with.
The 7-Stage Scale of Alzheimer’s
One of the most commonly used scales is the 7-stage scale, often referred to as the Reisberg Scale, or GDS (short for Global Deterioration Scale for Assessment of Primary Degenerative Dementia). The GDS scale divides the disease process into seven stages based on the amount of cognitive decline in the inflicted senior.
What to Expect
In the early stages, Alzheimer’s disease can interfere with day-to-day tasks; while in the later stages, someone with Alzheimer’s will depend entirely on others to complete basic tasks. The seven stages associated with this condition are as follows:
Stage 1: No Cognitive Decline
In this stage (really a pre-stage), a person may simply know about the risk for Alzheimer’s disease due to family history. Or a doctor may identify biomarkers that indicate risk. But there will be no noticeable symptoms during the first stage, which can last for years or decades.
Duration: N/A
Care: Someone in this pre-stage should do what he can to stave off Alzheimer’s for as long as possible. Consider the following healthy habits:
- Exercise: The most convincing evidence is that physical exercise helps prevent the development of Alzheimer’s or slow the progression in people who have symptoms. The recommendation is 30 minutes of moderately vigorous aerobic exercise, three to four days per week.
- Eat a Mediterranean diet: This has been shown to help thwart Alzheimer’s or slow its progression. The diet includes fresh vegetables and fruits; whole grains; olive oil; nuts; legumes; fish; moderate amounts of poultry, eggs, and dairy; moderate amounts of red wine; and red meat only sparingly.
- Get enough sleep: Growing evidence suggests that improved sleep can help stave off Alzheimer’s. Aim for seven to eight hours per night.
Other recommendations include learning new skills, making social connections, and drinking less alcohol. Read our blog post, “How to Stave Off Dementia” for more details.
Stage 2: Very Mild Cognitive Decline
This stage is used to describe mild forgetfulness. For example, forgetting names and where familiar objects were left. Symptoms of dementia are not evident to the individual’s loved ones or their physician.
Duration: Unknown
Care: See stage 3 below.
Stage 3: Mild Cognitive Decline
This stage includes increased forgetfulness, slight difficulty concentrating, and decreased work performance. People may get lost more frequently or have difficulty finding the right words. At this stage, a person’s loved ones will begin to notice a cognitive decline.
Average duration of this stage is between 2 years and 7 years.
Stage 2 and 3 Care
- Remind the person: Simple reminders of appointments and names of people may be needed.
- Develop coping strategies: Caregivers can also assist with coping strategies to help loved ones remain as independent as possible, such as writing out a daily to-do list and/or a schedule of when medications should be taken.
- Pay attention to safety: Safety should always be considered, and if there are any tasks that a person with early stage dementia cannot perform safely on his or her own, supervision and/or assistance should be provided.
- Estate planning / Lifecare Planning / Medicaid Planning: During this period is when many people first receive an official diagnosis of Alzheimer’s. As soon as the diagnosis is received, it’s critical to discuss and make decisions about the future. For example, it is vital to make an appointment with an experienced Elder Law attorney, such as myself, to put together a sound long-term care plan (to avoid going broke in connection with paying for long-term care costs), a comprehensive estate plan (to distribute assets upon death, ideally outside of the nightmare of probate), and an incapacity plan (to avoid the need for lifetime probate, which involves petitioning the court to have someone declared incompetent so that a guardian and conservator can be appointed by the court).
Stage 4: Moderate Cognitive Decline
This stage includes difficulty concentrating, decreased memory of recent events, and difficulties managing finances or traveling alone to new locations. People in this stage have trouble completing complex tasks efficiently or accurately and may be in denial about their symptoms. They may also start withdrawing from family or friends because socialization becomes difficult. At this stage, a physician can detect clear cognitive problems during a patient interview and exam.
Average duration of this stage is 2 years.
Care: See stage 5 below.
Stage 5: Moderately Severe Cognitive Decline
People in this stage have major memory deficiencies and need some assistance to complete their daily living activities (dressing, bathing, toileting, etc.). Memory loss is more prominent and may include major relevant aspects of current life. For example, people may not remember their address or phone number and may not know the time or day or where they are.
Average duration of this stage is 1.5 years.
Care for Stages 4 and 5
- Assistance with Activities of Daily Living: Initially, an individual may only need prompts or cues to perform activities of daily living, such as reminders of the need to shower, or appropriate clothes laid out on the bed. However, at some point, more hands on assistance will be required.
- Establishing a routine becomes important and caregivers need to exercise patience.
- Clear communication: Since individuals in this stage of dementia have greater difficulty communicating, caregivers need to talk slowly, clearly, and at times, use non-verbal communication.
- Transportation assistance needed: Individuals will no longer be able to drive, so transportation assistance will be required.
- Supervision is necessary: It is in this stage of dementia when it becomes no longer safe to leave the individual alone, which means round-the-clock supervision is needed, either at home, in an Assisted Living Facility, or in a Nursing Home. This is when care can start to get very expensive, and it is important to keep in mind that Medicaid will pay for nursing home care (or, in most states, nursing home level of care provided at home), but will not pay for care provided in an Assisted Living Facility (ALF), even for someone in the memory care unit of an ALF.
Stage 6: Severe Cognitive Decline
People in Stage 6 require extensive assistance to carry out their Activities of Daily Living. They start to forget names of close family members and have little memory of recent events. Many people can remember only some details of earlier life. Individuals also have difficulty counting down from 10 and finishing tasks. Incontinence is a problem in this stage. Ability to speak declines. Personality /emotional changes, such as delusions, compulsions, or anxiety and agitation may occur.
Average duration of this stage is 2.5 years
Care: See Stage 7
Stage 7: Very Severe Cognitive Decline
People in this stage have essentially no ability to speak or communicate. They require assistance with most or all activities of daily living. They often lose major motor skills (e.g. the ability to walk).
Average duration of this stage is 1.5 to 2.5 years.
Care
- 24/7 supervision and care: A person in this last stage of dementia requires a significant amount of personal care and assistance, and round-the-clock supervision is needed, usually in a memory care unit of an Assisted Living Facility, or in a Nursing Home.
- Constant assistance: Dementia patients may require assistance getting in and out of bed, moving from the bed to a chair, or may even be bedridden and require help moving positions to avoid bedsores. At some point, the individual will be 100% dependent on his or her caregiver and will no longer be able to complete any daily living activities independently.
- Issues with swallowing: Swallowing becomes an issue in late stage dementia, and caregivers have to make sure food is cut into small pieces, or is soft, such as yogurt and applesauce, or is pureed.
There’s no cure yet for Alzheimer’s, but treatment and interventions can help slow the progression. By knowing what to expect from each stage, you can be better prepared for what is to come.
Planning for a Loved One with Alzheimer’s
Persons with Alzheimer’s disease and their families face special legal and financial needs. Controlling the high costs of caring for a loved one with Alzheimer’s, and navigating the emotionally and physically demanding requirements of caregiving, require the assistance of a highly skilled and specialized expert in the field of Alzheimer’s Planning.
At the Farr Law Firm, we are dedicated to easing the financial and emotional burden on those suffering from dementia and their loved ones. Through the process of Life Care Planning and Medicaid Planning (also-called Medicaid asset protection planning), we help protect a family’s hard-earned assets while maintaining your loved one’s comfort, dignity, and quality of life by ensuring eligibility for critical government benefits such as Medicaid and Veterans Aid and Attendance. If your family is facing a diagnosis of Alzheimer’s disease or any other type of dementia, please call us as soon as possible to make an appointment for a consultation:
Medicaid Planning Fairfax, VA: 703-691-1888
Medicaid Planning Fredericksburg, VA: 540-479-1435
Medicaid Planning Rockville, MD: 301-519-8041
Medicaid Planning Washington, DC: 202-587-2797












